<< Return to Hurricanes and Disaster Preparatio>
A Word or Two about Gardening: Biohazards in the yard: Playing it safe
By: John McLaughlin, March 27, 2005.
Playing it safe in the yard not only encompasses how to use garden implements and chemicals, but an awareness of various biohazards present in the yard. These latter include insect/animal bites, poisonous plants and the risk of infectious disease. It is the latter item that concerns this article. Yard work can expose us to four types of pathogens:
Bacteria, unicellular microorganisms differing from animal cells in not having their DNA in a cell nucleus (a conspicuous membrane bound structure). Another difference, the rigid outer bacterial cell envelope, is especially significant as it plays a major role in determining virulence. Some soil inhabiting bacteria can form extremely resilient spores, whilst many of those causing intestinal disease can be destroyed by elevated temperatures. This is an important consideration when making compost. While bacteria are important human, animal and plant pathogens, the vast majority are harmless, a vital part of sustaining life on earth.
Protozoa are also unicellular, but have more in common with animal cells. There are about 66,000 known species of which 10,000 are parasites. Well known protozoan parasites of humans include those causing malaria and sleeping sickness. Others are parasites of livestock (e.g., babesiosis), insects (Nosema in grasshoppers, used in Nolo bait, and Ophryocystis responsible for declining numbers of monarch butterflies) and even plants (Phytomonas in tomatoes, corn, coffee, bananas etc.). The present concern is contamination of garden soil by protozoan parasites dispersed in animal feces as resilient cysts.
Flat worms/tapeworms and roundworms are two groups of simple multicellular organisms that are important parasites of humans/animals, often with complex life cycles, usually involving two or more hosts, and/or an extensive migratory phase within the final host. In the yard, roundworms are of most interest, those passed in animal stools (as eggs, viable in soil for up to a year) or infective larvae (viability limited to several days).
Viruses infective to humans are not usually found in animal waste - bird flu is an important exception. Human waste is a definite hazard (enteric viruses), though not normally a risk when gardening except in exceptional circumstances. After inundation with sewage contaminated water, soil could remain contaminated for several days depending on temperature and rainfall. Of more immediate concern for gardeners are viral diseases spread by arthropod vectors, principally mosquitoes (e.g., West Nile Virus (WNV). Viruses have no cellular structure - in essence they are made up of a nucleic acid core surrounded by a protein shell/envelope. Even more elemental prions (protein particles) are the causative agent of bovine spongiform encephalitis (‘mad cow’ disease) and linked to variant Creutzfeld Jacob disease (vCJD) in humans. For gardeners the issue is the risk of using animal bye-products (notably bone meal) as a soil amendment. According to CDC , US steamed bone meal supplies are not regarded as posing a risk (destruction of prions requires steam sterilizing at 132ºC for 4½ hours).
Fungi are more important as plant pathogens, with few of the more than 100,000 known species being pathogenic for humans. The diseases (mycoses) they cause can be serious, especially for those with a compromised immune system. Fungi share certain features with plant cells, but lack chlorophyll and have a cell wall composed of chitin-like polysaccharides rather than the cellulose found in plants. They are found as either unicellular yeast cells or multi-cellular filaments (hyphae), and produce spores by both sexual and asexual processes.
It is possible to identify four main sources of infection in the yard:
Soil – contains naturally occurring bacteria and fungi which can cause disease (e.g., tetanus, botulism, histoplasmosis)
Animal waste – both wild and domesticated, pathogens in the latter instance often deliberately introduced to a site in raw or improperly composted manure. This could potentially contaminate soil and ground water with both bacterial and/or protozoan pathogens. Waste from wild animals and birds (especially pigeons and gulls) are potential sources of contamination. Reptiles (lizards, snakes etc) are a well known source of Salmonella (cause gastroenteritis). Diseases spread from animals to humans are termed zoonotic.
Plants – two routes of infection, consumption of improperly washed plant foodstuffs contaminated with pathogens (from soil/animal waste) or inoculation of organisms present on plant surfaces as a result of wounds from prickles or spines.
Animal vectors – passive transfer of pathogens from contaminated material (feces, carcass) on body surfaces of usually insects or birds, or by means of a biologic vector essential for development of the pathogen (mosquito and West Nile virus).
Animal bites don’t quite fit into any of the above. Apart from physical injury, bites from either wild or domesticated animals can become infected with resulting illness.
What specific measures can be taken to reduce biohazards in the yard? One simple precaution concerns manure, which should never be used raw – apart from health concerns, it can burn plant roots. When composted, manure has to reach temperatures above 140ºF for at least 5 days to ensure destruction of bacteria such as the potentially deadly 0157:H7 hemorrhagic strain of Escherichia coli. This bacterium causes severe disease, especially in children and is principally found in cattle manure. Most home compost piles are unlikely to reach sufficiently high temperatures to destroy this and other pathogens found in animal manure. Many other bacterial/protozoan pathogens are present in animal manure. Since cow, sheep or pig manure is unavailable to most local homeowners, further elaboration of the risk is not necessary. In residential areas composting should be limited to plant and none-meat kitchen waste.
In Miami-Dade horse manure is available to a limited extent. It produces poorer quality compost, but is regarded as presenting a lower health risk. A soil bacterium, Rhodococcus equi, found in horse manure, is well documented as the cause of respiratory disease in foals. More recently it has become of increasing concern as the cause of a severe form of pneumonia in persons having a compromised immune system (AIDS, immuno-suppressive therapy etc.). Infection occurs through inhaling dust contaminated with dried manure (wet down dried soil).
Recent research also raises concerns about Giardia in horses. Only certain genetic sub groups of this protozoan parasite have been associated with human disease, and the presence of one of these has been identified in samples of horse manure. Giardia causes bloating, diarrhea and nausea, which can be especially protracted and debilitating in susceptible individuals. Dogs and cats are among other potential animal sources of human infection with Giardia. Last year Miami-Dade reported 246 cases; nationally there are 2 million cases annually most of which involve contaminated water, but CDC estimates 10% to be food borne.
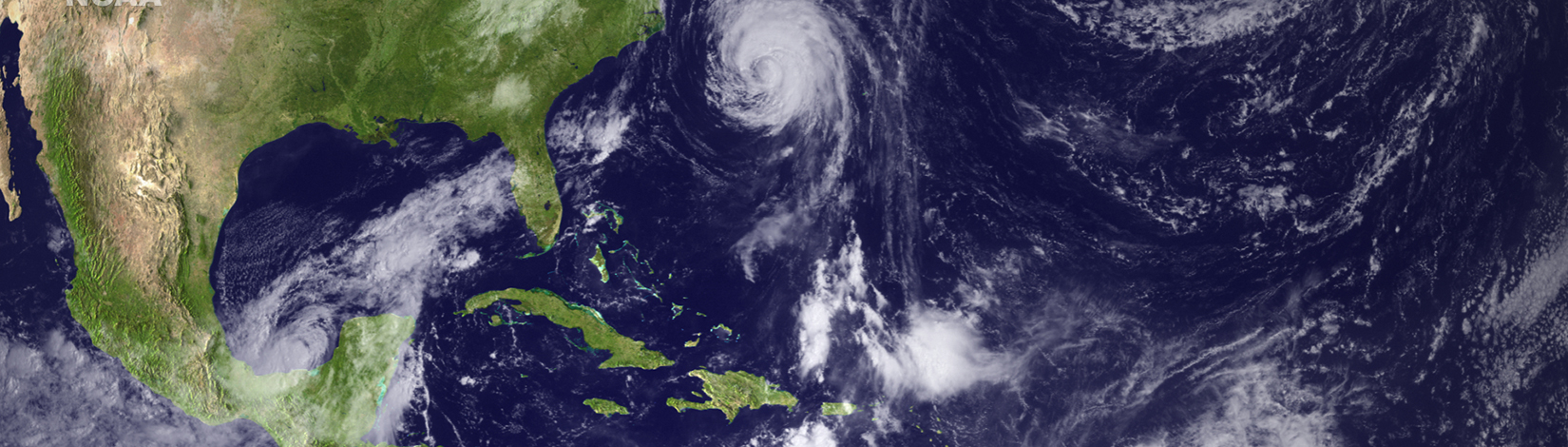
Flooded neighborhoods pose another risk when doing yard work – as after a storm. Of the myriad of bacterial pathogens that can be present in sewage contaminated flood water, Leptospirais of note since infection can occur via skin abrasions. Although cases are rare it can lead to hepatitis and kidney failure. Rats are the main reservoir, bacteria being passed in urine. Infection in dogs is on the increase nationally, especially in recently urbanized areas. Apart from Giardia, Cyclospora and Cryptosporidium are two other gut dwelling, water borne parasites found in Miami-Dade (26 and 37 cases respectively for 2004) that can cause severe diarrhea. Both form highly resistant cysts. Person to person spread of both parasites is important (zoonotic spread via calves can be significant for Cryptosporidia). Apart from some inconclusive evidence concerning dogs, it is the sole route for Cyclospora. Dogs and cats are far more important in the spread of several other parasites that can contaminate soil year round.
Reducing potential contamination of soil is a further area where we can be proactive. Toxoplasma is a protozoan parasite found in the small intestine of cats, the sole definitive host. The parasite is shed in cat feces as millions of resilient oocysts. Several mammalian species (including man) can act as intermediate hosts. When oocysts are ingested the parasite is released and migrates throughout the body and encysts in a range of tissues especially nerve and muscle. In developed countries human infection most often occurs through ingesting tissue cysts present in undercooked meat; however soil contaminated with oocysts from cat feces is recognized as an increasing risk. For two groups, those with a deficient immune system or pregnant women infection can be serious. In the latter case the parasite can cause loss of the unborn or a range of developmental problems for infants if undetected. For the rest of the population infection is usually asymptomatic - at most mild flu like symptoms (worldwide 30-50% of the population is believed to carry latent tissue cysts). Recently there has been increased recognition of more serious symptoms from severe lethargy to mental abnormalities. In this latter regard there are claims that sub-clinical infection with Toxoplasma contributes to development of schizophrenia.
Cats shed infective oocysts for at most 2-3 weeks and thereafter most are immune for life. Cats kept indoors, fed cooked meat products and unable to catch prey animals (e.g., mice) are at minimal risk of contracting Toxoplasma. Contamination of soil is mostly due to young, especially feral cats. If you have a children’s play area in the yard with a sand box, keep it covered. Never use the sand or spent cat litter as soil amendments. Toxoplasma oocysts once shed take 5 days to become infective, and can remain viable in soil for at least a year. Prompt removal of cat feces from the yard is a simple means of limiting contamination of soil. Dog and cat feces are also sources for two parasitic roundworms.
Removal of dog feces can reduce the spread of two roundworm parasites, one the cause of cutaneous larva migrans (creeping eruption, CLM) the other visceral larva migrans (VLM). The former is caused by the infective larvae of dog hookworms present in fresh dog feces. Larvae burrow through the skin, but in humans they are unable to complete their normal migration to the gut, and meander just below the skin where they produce serpentine tracks and intense itching. Survival of larvae in the soil is limited to a few days. More serious is VLM caused by Toxocaracanis, another intestinal roundworm of dogs (increasingly implicated is T. cati found in cats). Parasite ova are shed in the animal’s feces and can survive for up to 4 years in moist soil. On ingestion by a dog or cat infective eggs release larva, which penetrate the gut, migrate to the lungs where they are coughed up swallowed and return to the gut as adult worms. In humans the migratory phase never reaches the gut and larvae become localized in a range of organs including lungs, liver and kidney. This can cause various complications, one of the most serious being blindness if larvae migrate across the retina. This is most common in children and is usually associated with T. canis. The principal sources of infection are puppies (infected in utero) and pregnant dogs. De-worming pups can control spread of the parasite, but that still leaves stray animals as a source.
There are no chemicals, including lawn pesticides that will rid soil of roundworm or any other parasite eggs/larvae. Their use is a waste of money and only contributes to potential contamination of ground water. It takes at least 2 weeks for Toxacara eggs to embryonate (become infective) so again prompt removal of animal feces from the yard is an easy preventative measure.
As well as garden soil, potting soils and soil amendments can pose risks. Supposedly sterilized animal bye-products used in potting mixes gave been found to contain Salmonella. In the early 1990’s an Australian outbreak of legionnaire’s disease, normally associated with water cooled air conditioning installations, exhibited no point source of infection. The one factor common to all those infected was a keen interest in gardening. Subsequent investigation revealed the presence of the bacterium Legionella longbeachae in various Australian potting soils (more especially those containing composted leaves or wood rather than peat). In 2000 two cases of gardening related legionnaires disease were reported in the US , L. longbeachae being recovered from potting soil. More recently a separate gardening related source of Legionella was identified, aerosolized water from irrigation sprinklers. In both instances the disease risk appears low, but again susceptible individuals should take adequate precautions (face mask) when working with potting mixes.
Sphagnum peat moss has been implicated in cases of sporotrichosis, a fungal infection due to Sporothrix schenkii found in soil and on plant surfaces. The fungus gains entry via skin abrasions causes a hard nodule which darkens and ulcerates. This has been mistaken for the bite of the brown recluse spider, which is not indigenous to Florida . In persons with a weakened immune response the disease can become disseminated and is recognized as a complication of AIDS. Several years ago an outbreak in a Florida nursery was linked to dried sphagnum moss. Infection is also associated with plants having spines or prickles, and has been referred to in the past as “alcoholic rose gardeners’ syndrome” since many of the reported cases have been affluent, middle aged, white male gardeners with a drinking problem. It is prudent not to work with dried sphagnum if you have cuts or skin abrasions, otherwise wear a long sleeved shirt and gloves. Opportunistic infections involving other fungi, some well known plant pathogens (Bipolaris, Fusarium and Alternaria) are of increasing concern in cases of immuno-deficiency. For most gardeners fungi are most likely to be an indirect cause of illness due to inhalation of released toxic/allergenic compounds.
Preventing insect and animal bites can protect you from contracting disease. The threat from mosquito born diseases, principally due to West Nile virus, can be reduced if you eliminate areas of standing water – this includes everything from an old tire to the base of a bromeliad. Try to avoid gardening in the rainy season just before sunset or after sunrise when mosquitoes are most active. In Florida there is a definite link between a prolonged drought in spring followed by normal summer rain and WN epidemics. In summer a dry spell of 10 days or more followed by heavy rain (≈2”) increases the mosquito’s infectivity (mosquitoes do not take a blood meal in dry weather). The WN virus is not transmitted from person to person but only from infected birds and for a limited period (1-3 days post infection). Only 1% of those infected develop neurological symptoms, persons over age 50 being at most risk. However in some outbreaks polio like symptoms of paralysis were observed in those much younger and in apparent good health. An insect repellent containing 15% DEET applied directly to clothing (cotton, wool or nylon) or skin should be used. The CDC recommends also products containing picaridin for application to skin, especially for young children.
The two common ticks found in local yards are at the very least a nuisance but not as important as mosquitoes in vectoring human disease. The brown dog tick can become an indoor plague but rarely bites people and is not known to transmit human disease. The American dog tick bites humans, is only found outdoors and can transmit Rocky Mountain spotted fever (local cases rare). Lyme disease is seldom encountered in Miami-Dade (vectored by Ixodes species ticks).
Most people are familiar with the risk of rabies from wild animals (especially raccoons and foxes) as well as stray dogs. However the Florida Department of Health reports that rabies incidence in feral cats exceeds that in dogs. Any animal bite should receive medical attention – bacteria normally present in the animal’s mouth can cause infection (12-20% for dogs, up to 50% for cats).
For those persons at most risk: the very young, those with an impaired immune system due to disease (e.g., AIDS, diabetes, or alcoholism), chemotherapy, surgery (splenectomy) or age consider seeking advice from a health professional before gardening. Otherwise don’t become a hypochondriac when faced with yard work. Be alert to the risks, and follow the simple precautions listed above. This can help prevent discomfort, distress or even serious illness.